Waivers & Policies > Medicaid Waiver Programs > Waiver Application
Based on the Waiver’s program participant capacity (referred to as program slots) and funding available, the DDA can offer individuals the opportunity to apply to the Waiver program who are on the DDA Waiting List or in a specified reserved priorities noted in the approved waiver application.
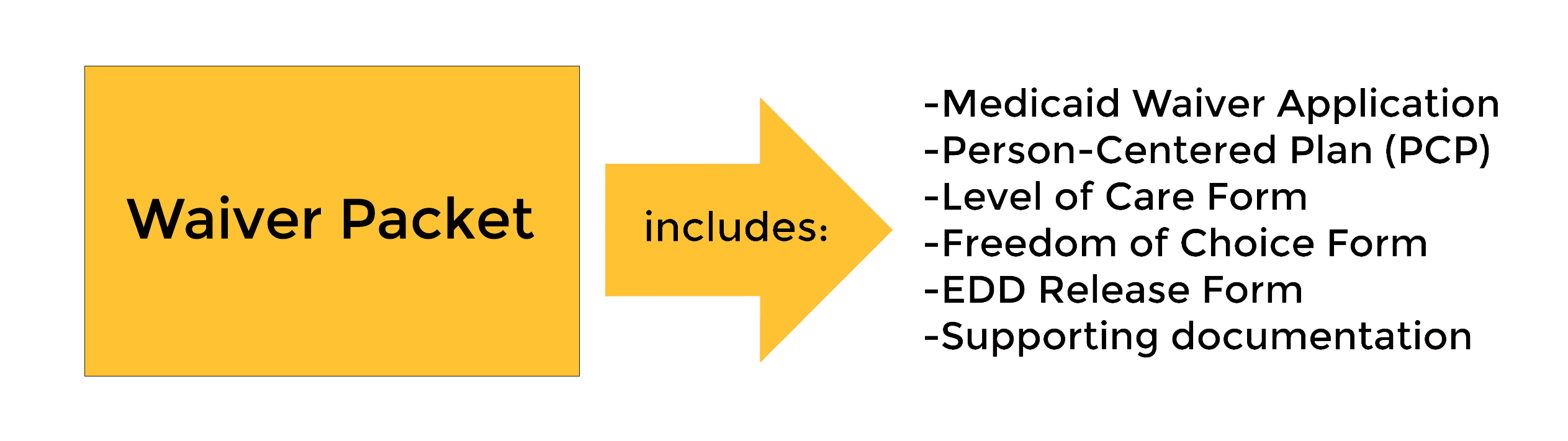
DDA Waiver Application Packet
A Coordinator of Community Services (CCS) will assist the person with completing the DDA Waiver application packet and exploring service delivery models, services, and provider options based on their assessed needs. Once completed, the CCS submits to the DDA regional office.
Waiver Eligibility Determination
The DDA
Regional Office
will assess the Waiver application and supporting documentation to determine if the applicant meets the technical and medical eligibility criteria in the approved Waiver. Technical eligibility includes but not limited to the applicant is a Maryland resident, determined to meet the DDA’s developmentally disabled eligibility criteria, and has an approved person-centered plan. Medical eligibility relates to meeting the institutional level of care of an Intermediate Care Facility for Individuals with Intellectual and Developmental Disabilities (ICF/IID). You do not have to go into an institution or agree to apply to an institution to apply to the waiver or receive services.
The Eligibility Determination Division (EDD) assesses Financial eligibility. They will review financial documents and databases to determine if the applicant meets the eligibility criteria. Applicants that meet all technical, medical, and financial criteria are enrolled in the Waiver.
The EDD sends an enrollment letter to the applicant and their authorized representative(s) informing them of the enrollment and effective date.
Applicants that do not meet all of technical, medical, and/or financial criteria are not enrolled in the Waiver. The EDD sends a denial letter to the applicant and their authorized representative(s) informing them of the denial along with appeal rights.
Important to note:
-
To determine financial eligibility, financial documents such as bank statements, assets, trusts, etc. are required for the applicant only. The DDA Waivers financial eligibility does not consider the income or assets of the family.
-
Participants must initially and annually meet all eligibility requirements. This includes submitting annual or updated financial statements and documentation, completing an annual person-centered plan, and being recertified to meet the medical level of care.
-
Once enrolled in a Waiver program, the participant can access
Maryland HealthChoice Program
service based on assessed needs.
-
Children are entitled to Medicaid’s
Early Periodic Screening Diagnosis and Treatment
services.

